Physiology
Many of us are familiar with the concept of homeostasis from introductory biology. This core concept is related directly to the physiology and etiology of diabetes. Several key chemicals, organs and hormones are involved in the process.
| Pancreas-Located on the left side of the abdomen, this important organ upholds the exocrine function of digestive enzyme production and the endocrine function of glucose-regulating hormones; most notably insulin (from the beta cells) and glucagon (from the alpha cells). The pancreas also creates somatostatin (delta cells) and pancreatic polypeptide (PPP) (F cells); although their function is currently unknown. | |
| Liver- | |
| Kidneys-In diabetes, excess glucose can be released through the kidneys, causing not only frequent urination, but also excessively "sweet" urine. The presence of such is one of the most common symptoms of diabetes. |
(Source: health.howstuffworks.com/ diabetes1.htm) Homeostatic balance of insulin and glucagon. (Source: health.howstuffworks.com/ diabetes1.htm)
| Glucose-A simple sugar (6 carbon monosaccharide) often broken down and utilized for energy by the cells of the body. Glucose is broken down into pyruvate during glycolysis, in which energy is released from the molecules. | |
| Glycogen-Many strands of glucose are transformed into this polysaccharide to store excess glucose in liver and muscles. | |
| Insulin-A hormone produced by the beta cells of the pancreas in the islets of langerhans. Beta cells account for 70-90% of all pancreatic cells. Insulin promotes the uptake of glucose in the cells, thus reducing the amount of glucose in the blood. Insulin also promotes lipogenesis (production of fat from extra glucose); protein accumulation in liver, fat and muscle tissue; and platelet activity (blood is thicker and chance of clotting increases.) Usually released after a meal to maintain blood glucose levels. | |
| Glucagon-A hormone also created by the pancreas in the islets of langerhans, but by alpha cells. It upholds the opposite function of insulin, in that it stimulates the liver and muscles to break down glycogen into glucose, which is then secreted into the bloodstream. It also promotes gluconeogenesis in the liver and kidneys. Usually released between meals and while sleeping to maintain blood glucose levels. | |
| Together Insulin and Glucagon work together to maintain a homeostatic balance in the body. |
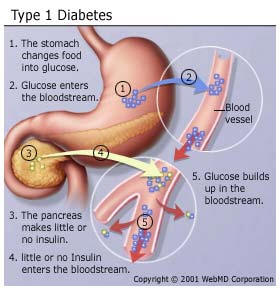
| In Type I diabetes, insulin is unable to regulate blood glucose levels due to the destruction of pancreatic beta cells, possibly by the body's own immune system. | |
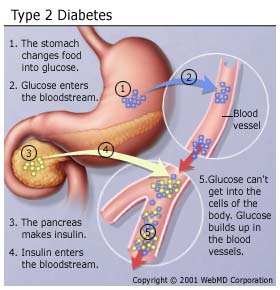
| In Type II diabetes, the body does not respond to an imbalance, cannot use own insulin, or is resistant to its effects. To compensate, the pancreas releases more insulin, which continues to be relatively ineffective. Resistance to insulin builds up consistently over time, worsening the condition. |
Etiology
![]()
| As stated before, the exact cause of Type I Diabetes is unknown. It is true that Type I Diabetes Mellitus is an autoimmune disorder which causes the immune system of the body to kill the pancreatic beta cells which produce insulin; however it can only be theorized at this point that a combination of autoimmune, genetic, and environmental factors (and possibly even viruses) contribute to the onset of Type I. | |
| The exact cause of Type II diabetes is relatively unknown as well; however it was been noted that those who are overweight and live sedentary lifestyles or more apt to develop Type II diabetes. Also, those with pre-diabetics are able to delay or prevent the onset of full Type II diabetes by changes in diet and exercise habits. Very rarely does Type II diabetes develop in children, but it also has been noted that in such cases where it does occur, the child is generally obese, from a high-risk ethnic group, and a family history of diabetes is present. This is perhaps due to the fact that glucose metabolism is highly heriditary. | |
| In gestational diabetes, the temporary disease can be attributed to the elevated estrogen levels that may also impair glucose metabolism. However, the presence of gestational diabetes indicates that the woman is at a high risk to develop Type II diabetes. |
Major Risk Factors in Type II Diabetes Development:
| Obesity (BMI index greater than 27) | |
| Over 45 years of age | |
| Family History | |
| Race (seen most commonly in Native Americans, Pacific Islanders, South Asians, Hispanics.) | |
| Giving birth to a large baby (over 9 lbs. at birth) | |
| HDL (high density liproteins) above 35 mg/dL | |
| TGL (triglycerides) above 250mg/dL | |
| HTN (hypertension=elevated blood pressure) above 140/90. | |
| Low socioeconomic status |
(Source: http://npgibson.com/classes/diabetes/epidemiology/riskfactors.htm)