Osteomyelitis In-depth
Etiology
Epidemiology
-
Non-specific Infection
-
Numerous reports show that 90% of
cases of osteomyelitis are caused by Staphylococcus
aureus.
-
The remaining 10% are due to: Streptococci,
Pneumococci, Meningococci, and Salmonella or Colon bacilli
-
Osteomyelitis can occur at any point in ones
life but it more often occurs between the ages of three and fifteen years,
which is the period of most active bone growth.
-
Osteomyelitis affects males more than females
by a ratio of 3:1.
-
Osteomyelitis typically affects long
bones.[2]
Types of Osteomyelitis
Bone Distribution (click image)
 [2]
[2]
Pathogenesis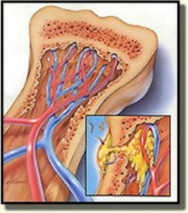 (click image)
(click image)
Morphological Characteristics
Note: Not all cases show all characteristics of
Osteomyelitis
Treatments