Table of Contents
2. Comparison between American and Japanese Medical Education-2000
4. My personal thoughts about Japanese medical education and health care-1997
5. Physical examination (PE) skills of first year residents
6. Ideal skills for junior residents(JR)
7. Creative Thinking-Clinical Problem Solving Resident Physician Training program Kameda Medical Center-1995
8. Clinical Rounds.: Website URL:-1996-1999
1. Stein G.H., Improvements of Japanese Surgical Training for the 21st Century: Problems and Suggestions Based on my 7 Years Teaching Basic Bedside Skills in Japan. Journal of Japanese College of Surgeons 2001. 26:14-19
ABSTRACT
The application of the methods of problem-oriented system and
problem-based learning are essential tools for teaching surgically
oriented Japanese physicians-in-training the clinical skills to
understand and manage their patients' problems independently.
Much time is needed during the first post graduate year in order
for these young physicians to become proficient in patient analysis.
The use of pre-printed worksheets and detailed repetitive medical
chart review with immediate corrective feedback, coupled with
bedside practical examinations and discussions, facilitate acquisition
of needed clinical skills. Surgical trainees need these basic
cognitive skills if they are to develop the proper skills for
understanding pre- and post- procedural invasive interventions.
Additionally surgical training should include the use of medical
literature for evidence based decision making as well as communicative
skills for talking with patients and families. These patient oriented
discussions should be in conformity with international ethical
standards. Future computerized patient interactions will require
surgeons to accept new models of clinical involvement. Life-long
continuous medical education will be essential as these new
technologies
are introduced. Young surgeons will lead the changes; old surgeons
will have to adopt the new methods or retire.
Key words: Japanese medical education, surgical
residency,
clinical skills, problem oriented system POS
Getting Started in Japan
After practicing and teaching clinical medicine for 22 years in the Department of Medicine, College of Medicine, University of Florida, Gainesville Florida, USA, I embarked on a teaching career in Japan, initially at the invitation of Dr. Tadashi Matsumura, Maizuru Municipal Hospital. While short-term teaching in Maizuru City, I received a invitation for a permanent position at Kameda General Hospital in Chiba Ken and remained there for 7 years as director of medical education and professor-in-residence. While at Kameda General Hospital I regularly consulted with many other medical facilities, such as Shonan Kamakura Hospital, Okinawa Chubu Hospital, St. Luke's International Hospital, Chiba University Hospital (2nd Department of Medicine), and US Naval Hospitals in Okinawa and Yokosuka. Varied bedside teaching experiences in these hospitals enabled me to develop a method of teaching young Japanese physicians basic clinical skills, based on the Problem Oriented System, used thought out US Medical schools for the past 30 years, which I modified for the Japanese medical educational system.
It is important for all graduating medical students and clinical residents to have these basic clinical skills for their further development as independently thinking and competent clinicians, regardless of their intended field of specialization.[1]
Problem Oriented System(POS) and Problem Based Learning(PBL)
POS refers to physicians' systematic method of organizing clinical data in order to understand patients' medical illnesses from each patient's medical history, physical examination, and laboratory data, permitting the physician to construct an individualized assessment and plan.[2] PBL is a similar systematic learning method based on the POS, used by medical students in tutorial group discussions, in which students discuss clinical cases from notes prepared by the tutor, who is characteristically a senior physician.
With either method, the student or resident organizes the clinical data, identifies the problems by creating a problem list from the history, physical examination, and laboratory data. The problems are grouped to form assessments which include likely diagnoses and differential diagnoses. The plan of studies and treatment must show that the student is following medical logic by supporting the plan from the assessment which in turn is supported by the history, physical examination, and laboratory data.[3] Learning involves using the students' accumulated fund of medical knowledge and finding published information to fully support their assessments. Self study from handbook and textbook assist the students in building their own database of medical facts to apply to the clinical problems.
Identifying Residents' Clinical Skills
As my teaching experiences expanded, I sensed the the need to evaluate residents' basic clinical skills in a systematic fashion. However, because of my rudimentary Japanese language skills, I was unable to assess residents' history taking from their patients[4]. Hence I focused on residents' physical examination skills, which I could readily observe.
In that context, I set up a observational study at Kameda General Hospital, which was approved by their postgraduate medical educational committee. Each first-year resident was invited, then instructed to perform a complete physical examination on a patient within a 30 minute time limit. I observed their skills by marking each of 45 physical examination items on a standardized conventional check -list, as the resident performed the task, without regard to quality of the performance.[5] The first phase of the study, called the pre-test, was done during the first week of the 6 month internal medicine rotation. Corrective feedback for improving their skills as well as a copy of their check-list was given each resident. The post-test was a physical examination repeated on a different patient with the same time limit and check-list during the last week of the 6 month internal medicine rotation.
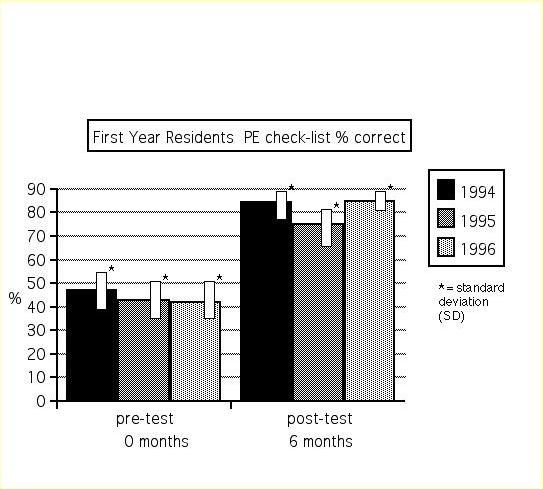
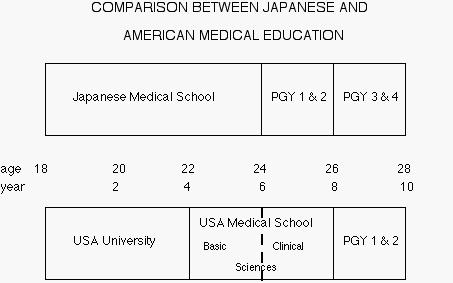
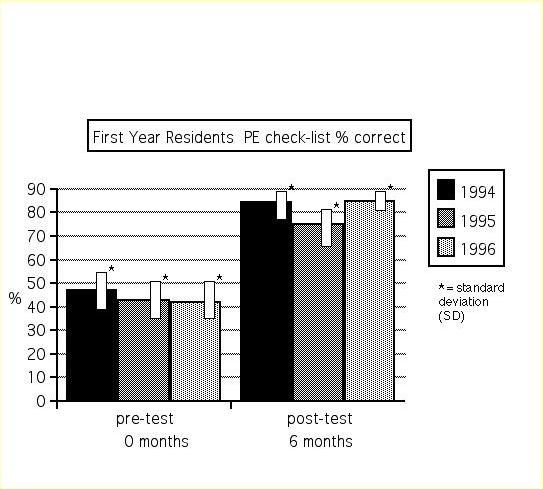
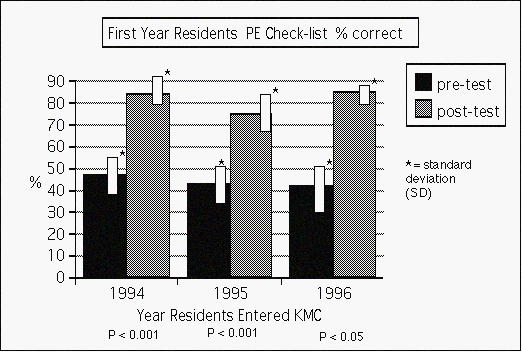
The results are shown in the Figure. Ten residents were observed for each of 3 years (10 residents multiplied by 3 years, or 30 residents in total). The pre-test results showed that the recently graduated medical students, now residents, performed about 45% of the items considered to be part of a usual physical examination. The post-test results showed that after 6 months of the internal medicine rotation, their performance rose to 80% of the items on the same check-list.
My conclusions of this quantity-identifying study (no attempt was made to asses the quality of the skill) was: 1) Entering 1st year residents have rudimentary physical examination skills; 2) Their skills improved by 100 % showing their ability to learn; 3) In comparison, US medical students are required to have a score of 90 % to pass a similarly observed physical examination check-list at the conclusion of the class[6].
On a daily basis I observed that their initial skills to use the POS for patient understanding was similarly poorly developed. Again I was unable to quantify these observations. I subsequently evolved a method of teaching the POS in spite of my poor Japanese language skills
Teaching POS: Setting
Instruction was held in a small conference room twice daily, each session lasting 1 1/2 hours 5 days each week for 2 months while the residents were on the general internal medicine rotation. Two to four junior residents discussed their cases with me as best they could using the POS method; each resident had about 2 new inpatients each week and managed 5-7 inpatients under my and the chief of service's supervision. Following the daily afternoon conference, bedside rounds were conducted for about 1 hour. Residents communicated in English, which in all cases improved during the 2 month interval. Their written case reports were usually in English since their English reading and writing skills were somewhat better than their conversational skills.
Teaching POS: New Inpatient Presentations
The residents were required to use pre-printed work sheets. The work sheets were developed from the standard University of Florida School of Medicine physical diagnosis class handbook by Akira Naito, MD, my former 2nd year Kameda General Hospital resident, under my supervision. Work sheets guided their data collection, showing them the needed data and providing a structure to formulate their problem list, assessment, and plan. The residents presented their cases the morning after the day of admission from the worksheets. This seemingly strict requirement enabled the staff to advance the work-up and management of the patient in a more orderly and expeditious fashion. In addition, residents were guided through their own interpretations of their patients' ECG's and imaging studies. During their case presentations I encouraged residents to support their assessments and plans from handbooks, textbooks, and at less frequent times, MEDLINE literature searches as a gentle introduction to evidence-based medicine. I lead the discussions with corrective feedback of information, praise and encouragement, requiring much patience on my part.
Teaching POS: Current Inpatient Presentations
The residents orally presented their current patients' progress from the patients' medical chart, using the exact S.O.A.P.[Subjective-history; Objective- focused physical examination and laboratory data; Assessment; and Plan] format. In addition the residents presented their assessment and plan at the bedside of each of their patients daily. This provided the opportunity for me to clarify the history and physical examination, thus providing direct corrective feedback to improve their bedside skills.
Teaching POS: Lectures
Lectures were limited in frequency to emphasize the importance for residents to focus on their own patients' problems, to perhaps 2-3 short lectures each week during the twice daily rounds. Journal articles were selected for practical common disease management, each resident being given a photocopy. Use of these articles served to emphasize the importance of using evidence-based medicine to make practical bedside decisions. Internet MEDLINE articles were similarly presented and discussed. Ethical issues were introduced as the patients' situations arose, including "informed consent" and "do not resuscitate" (DNR). Cultural issues, such as understanding differences of opinion between physicians, explaining other physicians' failure to use evidence-based medical literature for their decisions, and our own and other physicians' errors, were openly discussed.
Teaching POS: Personal Observations
I observed that, in general, entering first year residents, immediately after graduating from medical school, have inadequate basic clinical skills, lack confidence, or are overconfident, and are deficient in analytical problem solving ability. However, their skills dramatically improved during an intense 2 month training, surpassing the skills of senior residents who have not received interactive POS training. The use of worksheets permitted the residents to know the expected and needed data to compile a problem list, assessment, and plan. Corrective feedback of information and praise encouraged residents to ask questions and seek their own answers, a process of interactive learning. Patience was essential; each resident learned at a different rate, some quickly, others slowly. I felt it was necessary for residents to hear that I, as surely is the case with all senior physicians, have incomplete medical knowledge, uncertainties, and insecurities with some of my medical decisions. Residents observed me seeking firmer basis to finalize decisions from consultants and literature searches when uncertainties occurred.
Teaching POS: Conclusions
Concerning the POS, this method, when properly implemented with 2 months of intensive study, dramatically improved the inadequate clinical skills on first year residents. Daily recitations and bedside presentations by residents of each patients' problems enhanced acquisition of basic clinical skills. Corrective informational feedback and personal encouragement developed correct levels of confidence and independent problem solving skills. A successful clinical instructor needs to interactively focus on teaching clinical skills and be very patient as the resident slowly matures into a trained physician. I also suggest instructors reveal their uncertainties and insecurities. When these occur, they might increase their use of consultants and literature searches.
Teaching POS: Application to Surgical training
Surgical residents need problem-solving skills just as all clinicians need these skills, without exception. Examples abound in every aspect of surgical care performed by surgical residents. I mention some of them here. A patient enters a local emergency room with abdominal pain. The surgical resident must think about the clinical findings via history and physical examination, make a problem list, then construct an assessment with differential diagnosis leading to the logical plan of studies and the plan of treatment. If surgery is considered, the indications for the operation must be specified, including the application of current clinical guidelines and/or critical pathways of patient management. Meticulous preoperative care is another learned application of POS, including fluid, blood pressure, fever, and prior medication management. When the resident's mind is fertile for creative thinking, interpretive solutions to unique situations during the surgery will lead to better surgical outcomes rather than rote techniques. Post-operative management is yet another application of POS, for residents to learn fluid balance, wound care, fever, etc. Surgical out-patient care when focused on problems, assessment and plan provides a logical framework for residents' education. Lastly, ethical considerations, such as informed consent for surgery and DNR for terminal cancer patients, need to be learned at every phase of patient management.
Surgical case illustrating POS
Perhaps a description of an actual surgical case might highlight the importance of the application of POS to surgical patient care. The plastic surgical patient case was kindly provided by surgeons Kenishi Arashiro, MD and Kunihiro Ishida, MD. Their patient was a middle aged man who was brought to the Okinawa Chubu Hospital emergency room with a large rail impaled through his face. The rarity of this injury necessitated that basic surgical principles be applied. These included stabilization of the patient by assessing the "ABC's" of airway, breathing and circulation. Trauma management is best performed by using the standardized algorithms for advanced traumatic life support(ATLS). These procedures are best learned in the POS format with simulated practice to affect the resuscitation smoothly. Creative thinking is necessary to conceptualize the detailed anatomy of the damaged structures. Thinking that the impalement might have impinged or perforated the carotid artery, the surgeons elected to leave the rail in place prior to its surgical removal. Also time for removal was perceived to be of essence which meant preoperative studies had to be minimal. A surgical resident might have done an Internet MEDLINE search on impalement injuries for guidance. Once the surgical removal had started, creative thinking was again necessary to preserve the damaged organs, blood vessels and nerves. Of course, dexterity skills were necessary for the successful outcome.
During the operative repairs, there is frequently time to instruct the resident in surgical principles involved in this case using the POS. The post-operative problems of fluid balance, electrolytes and fever are best learned by the POS. Lastly the ethical considerations of informed consent with the patient's family might have included the high risk of death and other complications from the removal of the rail. It is a credit to these skillful surgeons that their patient had a successful outcome, which they felt was mostly due to their strict adherence to basic surgical principles, again learned through POS.
Futuristic surgery
Change is occurring in every field of medicine, no less so in surgery. Building on the present, I predict the following changes will happen in the surgical field. Computer applications for the collection of patient data including history and laboratory results, with the generation of problem list, assessment and plan, will become commonplace, Computer simulated learning of surgical procedures will require residents to be facile with computer use. An increasing development of robotic surgery, guided by surgeons, will occur. Organ and stem-cell transplantation will have many more uses. Applications from the human genome project will change the nature and course of many common diseases, perhaps reducing the need for certain surgeries. Nanotechnologies will become useful surgical tools. An example of these microscopic devices might be a tiny item which removes atherosclerotic plaque from vessel walls. Another prediction is that patients will use computers to assist with the management of their chronic diseases, reducing their dependence on physicians. This trend is developing in many Western countries. I leave it to the readers' and science fiction writers to dream of further possibilities, some of which will undoubtedly come true.
Futuristic Surgical Training
The impact of these and other difficult-to-predict changes on surgical training might be the following: Basic clinical skills may be de-emphasized. However, clinical reasoning skills will retain their prime importance[7]. Computer skills and its applications will become an important component of training. Life-long continuous surgical education will be essential as these developing technologies are introduced into community surgical practice. Young surgeons will lead the changes; old surgeons will have to adopt the new methods or retire.
References
1. Kassirer, JP. Teaching problem-solving - how are we doing.
N Engl J Med 1995;332:1507-1508.
2. Weed LL. Medical records that guide and teach. N Engl J Med
1968;278:593-600 and 652-657.
3. Weed LL. The problem oriented record as a basic tool in medical
education, patient care and clinical research. Ann Clin
Res.1971;3:131-134.
4. Voytovich AE, Rippey RM. Knowledge, realism, and diagnostic
reasoning in a physical diagnosis course. J Med Edu 1982;57:461-467.
5. Bates B, Hoekelman RA. A Guide to Physical Examination. 6th
ed. Philadelphia: J.B.Lippincott, 1995.
6. Stein GH. Comparison between American and Japanese medical
education. Journal of Okinawa Chubu Hospital. 2000;26: 45-51.
7. Weed LL. Sounding Boards. Physicians of the future. N Engl
J Med 1981;304:903-907.
Figure Entering first year residents quantitative per cent correct physical examination items at the start (pre-test) and 6 months at the end (post-test) of the internal medicine rotation, performed over 3 years with 10 residents each year
2. Stein
G,H., Comparison between American and
Japanese Medical Education. Journal
of Okinawa Chubu Hospital 2000.269(1):45-51.
American Medical Education
Goals of American Medical Education: an improved method of clinical skill training
Outline
1. Development of basic clinical skills for logical thinking and
solving clinical problems
2. Integration of the basic sciences of human disease with clinical
medicine.
3. Interactions with junior and senior physicians and consultants.
4. Learning to use medical literature searches for clinical decisions
based on evidence.
5. Development of life-long learning patterns.
6. Participation in peer review and quality assurance.
7. Discussions of community ethical issues.
Details of logical problem solving: The first goal
The main goal of North American clinical training is the development of the basic clinical skills for medical student and residents to manage their sick patients independently. These basic clinical skills which are taught to each medical student include eliciting a useful focused complete medical history, performing a thorough physical examination and selecting the essential laboratory tests. Further the integration of this information, obtained from the patient and clinical laboratory, enables the medical student to formulate a problem list from which diagnosis emerge. This method may be called S.O.A.P. [Subjective (medical history), Objective (physical examination and laboratory data), Assessment (diagnosis) and Plan(further studies and treatment)] or P.O.S. (Problem Oriented System).
As the patient's clinical course progresses, the medical student becomes skillful in altering the problem list with changing assessments and clinical plans to improve the patient's management and outcome. I may use the terms medical student and resident interchangeably. since there is overlap of these positions in Japan. Hence these creative problem solving skills are taught each medical student/resident with one patient at a time. These abilities are necessary because each patient is unique. This uniqueness and variability between patients with the same disease must be fully understood if the medical student/resident is to successfully grasp and manage the clinical problems of his patient. Independent thinking can be learned by each medical student/resident. Dependence on senior physicians for answers to clinical problems will inhibit their development. Each trainee must learn to think for himself and to find the answers himself.
Perhaps selected details of these skills might be helpful. Firstly regarding history taking, the incorporation of the review of systems(ROS) specific for each problem of the present illness permits the resident to literally learn about the disease from the patient. In some cases this might mean that the medical student/resident must read about the probable diagnosis in a standard textbook of medicine to learn the important questions to ask the patient, then return to the patient's bedside for further history taking. Also medical students/residents are required to ask most of the questions from a standard ROS listings. Secondary patient problems are uncovered frequently by this method. Further, residents are shown how to review hospital charts of prior admissions for complete data retrieval. They are instructed in techniques for telephoning community physicians for greater data input. These refinements enable the medical student/resident to have complete subjective data about his patients.
Regarding the so called objective component of clinical skills, namely the physical examination, there is a special emphasis: the psychophysical skills of finger and ear training, that is, palpation, percussion, and auscultation. Frequent bedside demonstrations of patients with cardiac murmurs, organomegaly, neurologic signs, arthritic joint limitation, etc., enable the medical student/resident to acquire these important skills. Routine laboratory data are analyzed for significance of both normal and abnormal results. The medical student/ resident then formulates a problem list, writing down every important item from the subjective and objective data base. Related problems are grouped together. From the reorganized problem list the assessment list is developed, fully integrating the clinical data into a useful and prioritized understanding of the actual clinical situations. The plan of needed studies to support the evident as well as the differential diagnosis is then developed. Readings in medical textbooks and consultations with specialists are encouraged. Lastly the plan of treatment, with drugs or surgical intervention, is discussed.
Hence the tool needed to understand the initial evaluation of the patient, namely the S.O.A.P. method, is slowly taught each medical student/resident, one at a time, over a 2~4 year period. The instruction takes place on a small conference room and at the bedside of the patient. As the resident presents his/her patient, he/she is guided supportingly through the S.O.A.P. steps. The resident is assisted with further history questioning of the patient for clarification of the illness and understanding the impact on the patient. At the bedside these further questions are asked and analyzed; the resident's hands on the patient are trained to feel correctly; ears on the stethoscope are tuned to hear gallop rhythms and murmurs. The patient's clinical course is followed closely. Each problem or assessment is understood within the S.O.A.P. format on a daily basis. This requires the resident to examine the patient and review the medical chart daily; progress notes using the S.O.A.P. system are encouraged. Immediate feedback of successful actions of the resident cultivate confidence in the newly acquired clinical skills. Other training methods include daily conferences and monthly morbidity and mortality conferences. Clinical procedures, from simple bedside ones to complex ones using the latest technologies and equipment are taught by competent staff. Residents receive frequent evaluations of their development and clinical skills to assist with their improvement and career choices.
Integration of the basic sciences of human disease with clinical medicine
Another goal of the training program is the integration of the basic sciences into clinical practice. The resident is continuously encouraged to keep asking why the particular clinical course developed. The usual medical model of antecedents, that is, what came before each event, and before that event, etc. is explained in pathophysiologic terms. By this method, there is a stimulation of medical curiosity to review applied aspects of anatomy, physiology, biochemistry, pathology, microbiology and pharmacology for each of the resident's patients.
Interactions with junior and senior physicians and consultants
Successful interactions between junior and senior physicians teaches mutual respect and helpful interdependency. It is a kind of team concept with each level of physicians teaching those lower in years of study. Those with longer years of experience, however, must keep an open mind to learn from their juniors, who may have newer information to contribute.
Learning to use medical literature for clinical decisions based on evidence
A recently developed technique for improved patient care is evidence based clinical practice. The basic concept is that physicians are trained to use the medical literature to support their decisions. Use of textbooks and computerized literature searches must be freely available to residents. Toward that goal residents at American teaching hospitals are learning how to use the library's data base via computer and textbook to support their clinical choices.
Development of life-long learning patterns
Such literature searches underscore the reality of continuously changing medical information. This should result in the resident's understanding that to practice contemporary medicine requires continuous life long devotion to reading the medical literature. An additional aspect of using these modern tools of contemporary medicine is the gentle challenge by residents to senior physicians who might have reached faulty conclusions based on outdated data.
Participation in peer review and quality assurance
Another topic is resident participation in peer review and quality assurance. These physician directed programs aim to improve patient care by analyzing physician management of selected problems. A possible example to illustrate peer review might be that physicians analyze medical charts of all patients dying from causes such as acute myocardial infarction or even unknown causes. If the causes of the death are not well evaluated or errors occurred in patient management, then the treating physician is required to explain his treatment plan. If his explanations are not satisfactory to his peer physicians, they may require him to take postgraduate medical education courses to improve his skills, or monitor his care of patients. Peers might even restrict his practice in extreme situations. Although this example is a hypothetical situation, it is similar to current medical practice in North America and parts of Western Europe.
Quality assurance(QA) is slightly different from peer review: more hospital wide indicators of quality of care are selected and analyzed. At American hospitals, QA programs are fully developed. For example surgeons are collecting data on their patients' return to the operating room for corrective surgery after the initial surgery. Another example is internists are collecting data on return of their patients to the intensive care unit following recent discharge from the I.C.U. Such data analysis should show physicians as well as nurses and administrators better ways of patient management.
Discussions of community ethical issue
A final topic that is the ethical understanding of patient care. Some of the areas of interest concern informed consent, that is, telling the patient what to expect from medications and procedures, both benefits and possible harm with poor outcomes. Further, residents are actively assisted with managing the patient and his/her family when death is approaching. Do not resuscitate(DNR) orders are fully explained to residents, nurses, and the patient's family.
Features of the American medical educational system
The reasons for ranking American medical educational system as one of the best in the world are as follows: Logical thinking method is the best way to understand comprehensively patient problems. Personal opinion and learning by watching and observation, the traditional methods of acquiring new skills, are less important in the American system. There residents and medical students are actively taught and closely supervised much greater than in many other developed countries. Teaching physicians enjoy discussions with residents about their patients; they bring current articles from the medical literature into the daily rounds. This 'evidence based' clinical medicine method insures that current information is applied to the patient's problems, that personal opinion is less important than published data, that senior physicians learn from junior physicians when such younger physicians have better information. Young physicians are urged to use and follow national consensus clinical guideline for patient diagnosis and management. Such use builds confidence among physicians. Physician arrogance mostly evolves from physician insecurities. The American teaching team aims to reduce both residents' arrogance and insecurities.
The group feelings are very different from those in Japan. In America all senior residents supervise junior residents. They do not have their 'own' patients as in Japan. Medical students (equivalent to first and second year residents in Japan) are supervised by their senior and junior residents. Senior physicians supervise all members of the team. Note however, independent logical problem solving is encouraged at every level. None may advance to the next year's higher level without proof of satisfactory performance. There is no automatic promotion. Those medical students and residents deficient in clinical skills are required to repeat the year and may be removed from the program. Hence as residents advance to the next higher level, they develops confidence in their clinical skills; they have passed practical tests; they have less insecurities and less need for arrogance. Also the practical aspect that senior physicians are regularly learning from junior physicians keeps the senior physicians from becoming arrogant while boosting the confidence that the junior physicians have meaningful contributions to make.
Differences between American and Japanese training
Another major difference between American and Japanese training programs is the pace of the workload. In America junior residents admit about 4 patient each day; the senior resident who is supervising 2-3 junior resident is responsible for 8-12 daily admissions. The work place has a rapid pace of evaluation and treatment of inpatients; the average length of stay is about 6 days. Residents are on call for emergency admissions every 4 th evening, night and weekend; they spend the entire night in the hospital, at times without sleep. For the 3 other evenings and weekends, they may 'sign out' to the on call team, leaving the hospital in the early evening. At many Japanese teaching hospitals, junior residents admit about 2 patient a week; senior residents about 4 patients a week. The length of stay is about 16 days. Senior residents may not supervise junior residents. There is no standard admission day; all days are admission days. There is no formal 'sign out' system; residents informally make their own arrangements. Residents have not been required to be in the hospital during the night. Most residents remain in the hospital until the late evening; even when they have no patient work they stay late to talk to other physicians and nurses to convey the group's sense of togetherness.
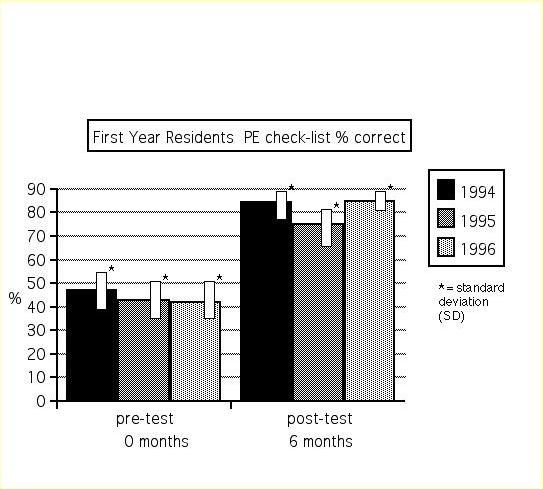
The implications of these differences may not be apparent. In the American system the residents have many patients in a short period of time. Clinical skills are learned rapidly, generally by 2 years in non-procedural programs. There is lots of stress for residents working in teaching hospitals. In Japanese teaching hospitals, the pace is more relaxed; there is much less stress for residents. However it takes a longer time to adequately develop clinical skills; it may take 2~3 extra years of post graduate training to equal the 2 years of American residency. Note that medical education in America requires 8 years of study for the M.D. degree, then 2-4 or more years of residency. In Japan medical students study for 6 years at the university, are awarded a MB (Bachelor of Medicine) degree; then they continue their residency training for minimum of 2 years, Some continue training for an unspecified duration, perhaps from 1 to 8 years additionally. An advanced medical science degree may be awarded during this interval for those enrolled in a university program. Hence the first two years of Japanese postgraduate medical education, that is, residency, should be considered equivalent to the last two years of American medical school.
Medical student differences
On a related topic American medical students attend all their classes. The lectures and related laboratories are very practically oriented. No one sleeps during lectures. Weekday evenings are spent studying. Weekend parties are small with modest amounts of alcohol consumption. Japanese medical students frequently do not attend lectures which are predominately related to the professor's research. The lectures are considered boring; many sleep during these times. There are frequent parties with much alcohol consumption. Of course there are exceptionally different students on both sides of the Pacific.
Medical chart differences
The patients' medical chart also reflect differences. All American physicians are required to have precise collection of patient data; detailed admission histories and physical examination, logical assessments and plans with at least daily complete logical progress notes. All medical charts are reviewed. Failure to comply results in penalties against the physician. Chart work is extremely important because it documents the physicians thinking processes and the exact patient course. In most Japanese hospitals, chart work may be required; it is rarely reviewed except for billing purposes. I know of no penalties for incomplete chart work , except, again, for billing purposes. A greater proportion of American hospitals use the computerized medical chart for history and physical examination recording as well as for progress notes
Advantages and disadvantages of the American and Japanese systems
On a related topic, I am frequently asked by medical students and residents to explain the differences and advantages of the American system of medical education., in two minutes or less. One the one hand, I tell them there is no advantage for them to aspire American residency training. This is because the Japanese medical education is a complete system, with training and life-long career practice relatively comfortable for the Japanese practioner. The Japanese health care system is focused on the physician in a paternalistic manner. Conformity to the group norms makes for a comfortable, stable practice environment, without threat of malpractice from irate patients. The Japanese educational framework from primary school through graduate education fosters discipline and obedience to authority; individuality and creative thinking are either discouraged or not overtly encouraged. On the other hand, the rigors of precise clinical problem solving skills are sub-optimal, errors in patient management are relatively frequent, harm to patients is overlooked without criticism or feedback to the practioner, medical chart work poorly documented, all resulting in many instances of both over and under treatment. Some exceptional Japanese teaching hospitals, such as Oaken Chub Hospital, as well as medical students and residents intrinsically recognize this dilemma and desire change and improvements.
The American system of medical education has been know for its openness to group discussions, sharing of ideas regardless of position or status and dedicated focus on the patient. Evidenced-based clinical decisions have power over personal opinions, even those of the professor. Accountability and a vigorous system of checks and balances enforces the patient- centered practice milieu. Problem solving skills and creative thinking are introduced in primary schools and enhanced throughout the maturation of the competent clinician. American medical practice requires a balance between the science of medicine(evidence-based data) and the art of medicine(caring and biomedical ethics). These listed advantages of the American system must be understood in the context of disadvantages. For example any physician may make a mistake. However, such errors in clinical judgment may bring stiff penalties in my country. The freedoms of independence and clinical practice are being limited these days by the necessities of curtailing the enormous national health care expenditure, currently 14-15% of gross domestic product (compared to about 7% in Japan). These financial limits are already impacting on postgraduate medical education in ways that are partially detrimental to residency training. Decreased length of hospital stay for in-patient care decreases total costs at the expense of decreasing the educational training benefits to residents. Residents are becoming mere overworked data managers with little time to think about and discuss their patients' problems. Managed care forces residents to attend to greater number of patients each day and week without comprehensive care for their needs. The prior years training balance between education and labor is shifting toward decreasing educational efforts and increasing toil. To add further difficulties to the burdensome resident's life, training programs are reducing the number of available residency positions while increasing the patient load. These reductions are occurring because of an over-supply of physicians. The brunt of these reductions will occur with international medical graduates(IMP) seeking training in America. Hence the opportunities for IMP to obtain American residencies are being restricted currently with greater limits planned for the future.
International medical graduate training in America
Because of the perceived successful Japanese
medical educational system by Japanese, and because of the generally
low level of English language speaking
skills, they have made up a very small percent of IMP in America.
The largest numbers of IMP are from India(20%), Pakistan(12%)
and the Philippines(9%). Japan is not among the top 10 countries
having participants in American postgraduate clinical training
programs.
In considering these advantages and disadvantages in the American system, Japanese young physicians should understand that no system is perfect, each has benefits and detriments. Yes, I clearly find many advantages to the Japanese system, as for example, its gentleness to colleagues, its forgiveness for physician errors and the security of its ikyoku system. But overall, there is no doubt in my mind of the superiority of the American medical educational system.
Advantages to remain in Japan for clinical training
Fortunately there exists a small but highly dedicated group of serious minded bright Japanese medical students, residents and senior physicians wanting to improve this deficient state of medical training and practice in Japan. It is to this small determined group that I devote my energies to support and encourage their struggles to understand analytic problem solving skills, the foundation of Western medical practice. For the average residents I have helped train at many Japanese teaching hospitals, I do not encourage them to study in American., for the reasons stated above. Rather it is my hope that through exposure to the American system as exemplified by Oaken Chub Hospital's successful medical educational programs, exposure to select Japanese national medical educational leaders, contact with Western trained medical educators, a growing number of Japanese physicians will have increasing influence to modify the tradition - bound restrictions inhibiting the proper development of clinical training and practice in Japan. These necessary modernization modifications include the field of biomedical ethics as well. The international medical communities have agreed that informed consent requires the end of the paternalistic physician role, supplanted by the decision control vested in the patient's (or his/her surrogate ) informed consent to all management and treatment issues.
Conclusion: Japan must improve clinical training
For a financially rich and developed county as Japan clearly is, with its internationally acclaimed automotive and electronics industries, its medical education and heath care practices are well below Western standards. I predict the aging of the population will force changes which I can only hope will improve clinical practice. The Japanese people deserve better care than is currently available. Okinawa Chubu Hospital is one of the facilities with a national reputation to lead improvements in Japanese health care into the 21 st century.
Biography of Gerald H. Stein, MD, FACP[in Japanese]
Dr. Stein, a native of Philadelphia, Pennsylvania, USA, graduated
from the University of Pennsylvania ,School of Medicine. After
two years of residency at the Boston City Hospital, Harvard Seervice,
he completed his clinical training for 3 additional years at the
University of Florida Teaching Hospital, Gainesville, Florida.
For the next 20 years he held several positions at that College
of Medicine. Tadashi Matsumura, MD, invited Dr. Stein to be visiting
professor at Maizuru Municipal Hospital in Kyoto ken. Shortly
thereafter the Kameda brothers invited Dr. Stein to teaching at
Kameda General Hospital. He acceepted the position as director
of medical education and professor-in-residency, which he held
for 7 years. During those years he was teaching consultant at
many Japanese hospitals including Chiba University Hospital, St.
Luke's Hospital, Shonan Kamakura Hospital, the American Naval
Hospital, Yokosuka, and Okinawa Chubu Hospital. He has lectured
at several Japanese teaching hospitals as well. Currently he is
visiting professor of general internal medicine, Okinawa Chubu
Hospital, and consultant Okinawa American Naval Hospital. His
faculty appointments are Associate Clinical Professor, University
of Hawaii and Courtesy Assistant Professor, University of Florida.
3. Stein, G.H., A Realistic Assessment about American Residency Training for Japanese Medical Students and Residents: My Four Years Teaching in a Japanese Hospital. In: Teruya, J., ed., A Guide to American Clinical Training: Practical Advice and Personal Experiences. Medical Sciences International, LTD. Tokyo 1997. p. 337-351
4. My personal thoughts about Japanese medical education
and health care
Noguchi Medical Research Institute
Annual Fellow Report, 12/97
Congratulations to Noguchi Medical Research Institute(NMRI) on
the conclusion of a most successful year. While I do not have
exact data of numbers of candidates participating in the various
programs, I have the feeling that the quantity and quality of
its new members have significantly increased. Further increases
are anticipated as the news about the exciting clinical training
opportunities are disseminated to Japanese medical schools and
teaching hospitals.
The recent availability of the facilities of the University of
Hawaii(UH) in Honolulu presents unique opportunities for Japanese
medical students and young physicians. The program launched this
fall, 1997, provides a complete American clinical experience under
the capable direction of Edward Morgan, MD, Associate Professor
and Director, Division of International, Department of Medicine,
University of Hawaii. NMRI's successful candidates have started
the month-long subinternship at Kuakini Medical Center. When the
candidate has adequate English language communication skills,
he/she is assigned patients for direct management under the supervision
of the medical staff. This means the participant writes orders
and plans the studies and treatments of the patient. In other
words, the subintern is not an observer but an active member of
the in-patient management team. Hence increased benefits of learning
clinical skills by 'hands-on' experiences enhances the value of
this training. In addition each subintern examines a patient under
direct observation of the ward team member both at entry into
the program and at its conclusion one month later. This 'clinical
skills examination' (CSE) includes an oral and written case
presentation
to the staff observer. The observer then makes a written critique
of the strengths and weaknesses for the subintern to see the
improvements
over the month and the areas needing further development.
I anticipate there will be helpful additions to the UH program
in the near future. Planned for implementation are drills for
brief clinical evaluations of simulated patients. These drills
should better prepare NMRI members for the soon to be required
clinical skills assessment for the ECFMG certificate, starting
7/98. Under preliminary discussion is the expansion of fields
of clinical study to include general surgery as the first offering
beyond general internal medicine. I hope other areas of clinical
medicine will be added thereafter to include pediatrics, OB/GYN,
and ER medicine.
Another aspiration I have for the future is for NMRI to increase
the number and scope of its goals for applicants. By this I mean
the greater number of participants in the UH program, the greater
the impact will be on Japanese medical education. The goal issue
is similarly important. Currently all successful NMRI candidates
must have a strong desire to try to enter American residency training.
That is a fine goal which I fully support. However, I am convinced
that a lesser goal should be considered, namely, to accept suitable
candidates whose goal is to experience the American health care
system as clinical clerks rather then as subinterns and not have
the immediate desire for American residency nor have taken or
plan to take the USMLE. Clinical clerks function as full members
of the managing ward team but have less responsibilities for their
patients; they may not write orders. Ideally these clinical clerks
will return to Japan wanting improvements in their medical educational
system.
On a related topic, I am frequently asked by medical students
visiting Kameda Medical Center to explain the differences and
advantages of the American system of medical education., in two
minutes or less. One the one hand, I tell them there is no advantage
for them to aspire American residency training. This is because
the Japanese medical education is a complete system, with training
and life-long career practice relatively comfortable for the Japanese
practioner. The Japanese health care system is focused on the
physician in a paternalistic manner. Conformity to the group norms
makes for a comfortable, stable practice environment, without
threat of malpractice from irate patients. The Japanese educational
framework from primary school through graduate education fosters
discipline and obedience to authority; individuality and creative
thinking are either discouraged or not overtly encouraged. On
the other hand, the rigors of precise clinical problem solving
skills are sub-optimal, errors in patient management are relatively
frequent, harm to patients is overlooked without criticism or
feedback to the practioner, medical chart work poorly documented,
all resulting in many instances of both over and under treatment.
Some exceptional medical students and residents intrinsically
recognize this dilemma and desire change and improvements.
The American system of medical education has been know for its
openness to group discussions, sharing of ideas regardless of
position or status and dedicated focus on the patient. Evidenced-based
clinical decisions have power over personal opinions, even those
of the professor. Accountability and a vigorous system of checks
and balances enforces the patient- centered practice milieu. Problem
solving skills and creative thinking are introduced in primary
schools and enhanced throughout the maturation of the competent
clinician. American medical practice requires a balance between
the science of medicine(evidence-based data) and the art of
medicine(caring
and biomedical ethics). These listed advantages of the American
system must be understood in the context of disadvantages. For
example any physician may make a mistake. However, such errors
in clinical judgment may bring stiff penalties in my country.
The freedoms of independence and clinical practice are being limited
these days by the necessities of curtailing the enormous national
health care expenditure, currently 13-14% of gross domestic product
(compared to about 7% in Japan). These limits are already impacting
on postgraduate medical education in ways that are partially
detrimental
to residency training. Decreased length of hospital stay for in-patient
care decreases total costs at the expense of decreasing the educational
training benefits to residents. Residents are becoming mere overworked
data managers with little time to think about and discuss their
patients' problems. Managed care forces residents to attend to
greater number of patients each day and week without comprehensive
care for their needs. The prior years training balance between
education and labor is shifting toward decreasing educational
efforts and increasing toil. To add further difficulties to the
burdensome resident's life, training programs are reducing the
number of available residency positions while increasing the patient
load. These reductions are occurring because of an over-supply
of physicians. The brunt of these reductions will occur with
international
medical graduates(IMG) seeking training in America. Hence the
opportunities for IMG to obtain American residencies are being
restricted currently with greater limits planned for the future.
Because of the perceived successful Japanese medical educational
system by Japanese, and because of the generally low level of
English language speaking
skills, they have made up a very small percent of IMG in America.
The largest numbers of IMG are from India(20%), Pakistan(12%)
and the Philippines(9%). Japan is not among the top 10 countries
having participants in American postgraduate clinical training
programs.
In considering these advantages and disadvantages in the American
system, Japanese young physicians should understand that no system
is perfect, each has benefits and detriments. Yes, I clearly find
many advantages to the Japanese system, as for example, its gentleness
to colleagues, its forgiveness for physician errors and the security
of its ikyoku system. But overall, there is no doubt in my mind
of the superiority of the American medical educational system.
Fortunately there exists a small but highly dedicated group of
serious minded bright Japanese medical students, residents and
senior physicians wanting to improve this deficient state of medical
training and practice in Japan. It is to this small determined
group that I devote my energies to support and encourage their
struggles to understand analytic problem solving skills, the foundation
of Western medical practice. For the average resident I help train
at Kameda Medical Center, I do not encourage them to study in
American., for the reasons stated above. Rather it is my hope
that through exposure to the American system as exemplified by
NMRI's successful medical exchange programs(both subinternships
and clinical clerkships), select Japanese national medical education
leaders, contact with me and similar Western trained medical educators,
a growing number of physicians will have increasing influence
to modify the tradition - bound restrictions inhibiting the proper
development of clinical training and practice in Japan. These
necessary modernization modifications include the field of biomedical
ethics as well. The international medical communities have agreed
that informed consent requires the end of the paternalistic physician
role, supplanted by the decision control vested in the patient's
(or his/her surrogate ) informed consent to all management and
treatment issues.
For a financially rich and developed county as Japan clearly is,
with its internationally acclaimed automotive and electronics
industries, its medical education and heath care practices are
well below Western standards. I predict the aging of the population
will force changes which I can only hope will improve clinical
practice. The Japanese people deserve better care than is currently
available. NMRI should be one of the national organizations leading
improvements in Japanese health care into the 21st century.
5 Stein, G.H.:Physical examination (PE) skills of first year residents. Proceeding:The 29th Japan Medical Education Society Meeting in Kanazawa,Japan, (July 1997).
ABSTRACT
Physical examination (PE) skills of PGY 1 Gerald
H. Stein, MD, FACP
Kameda Medical Center (KMC), Kamogawa City, Chiba Ken
[Object] Graduating medical students are assumed to have clinical
skills to perform an adequate PE upon entering the first year
of residency. The object of this study was to measure the quantitative
PE skills of entering first year residents and compare their scores
after completing 6 months of internal medicine rotations.
[Project design] All entering first year residents starting a
2 year super rotation at a non-university community teaching hospital
were invited to participate in the project. During the 1st to
2nd weeks in May, each resident performed a PE on one patient
within a 30 minute time limit. I observed each resident's PE,
checking off each of 45/47 (difference is breast PE in women)
items from a list as the resident performed the task. I modified
the check-list which I had used at the University of Florida (UF).
It is routinely used throughout American medical schools. The
original list contained 78 items. During the first year of the
study I standardized the check list to 45/47 items. In addition
to the pre-test during orientation, each 1st year resident received
a post- test at the end of the 6 month medicine rotation. The
post test occurred at 6 months for half of the residents and at
12 months for the other half.
[Results]For all the 22 residents(9 public medical schools 1 city
and 8 private ), the pre test scores were 11 to 30, with an average
score of 20 or 44 % correct. The post test scores were 27 to 44
with an average score of 38 or 82 % correct. The study was conducted
over 3 years. There was no apparent differences in the scores
between the 3 classes starting, 1994, 1995 and 1996. The 22 residents
used 55 % of the allotted time for the pre test and 78 % of the
allotted time for the post test.
[Discussion] Overall, graduating medical students performed less
than 50% of items on a simplified check list. The post internal
medicine rotation scores were about 82 %, indicating improvement
but suggestive of marginal clinical skills. Comparison score from
UF are 90 % required to pass; 0-2 failures/year. Possible reasons
for low proficiency include anxiety from being observed doing
PE first time, not using allotted time, and small sample size.
The KMC tests were scored for quantitative measures. Qualitative
assessment was not systametically evaluated. However I observed
most entering residents had poor techniques of percussion, palpation,
and auscultation. The order of the examination was often erratic.
[Conclusion] Japanese first year residents' PE skills are of
questionable
proficiency. Japanese medical educators might consider the significance
of these findings.
Physical Examination Skills
Objectives
1. Development of quantatative 'check-list'
for physical examination of internal
medicine in-patients by first year residents
2. Measurement of physical examination skills
of entering first year super-rotation
residents
3. Comparison of their scores after 6 months of internal medicine rotations.
Physical Examination Skills
Project Design
1. Modification of physical examination check-list,
from a standardized list used at the
University of Florida, Gainesville, Florida, USA. A similar list
is routinely used
throughout American medical schools to assess second year medical
students.
A. Reduction from 78 items to 45 or 47 items(difference is breast
examination in women)
B. First year development, standardizing, and testing of check-list.
This data
omitted from analysis since check-list frequently modified and
pattern of
scoring inconsistent.
2. Site of tests was Kameda Medical Center,
a 800 bed non-university private
community teaching hospital serving a rural community.
3. Subjects were entering first year residents of a 2 year super-rotation program.
4. Physical examinations were performed on
internal medicine cooperative in-patients,
within an announced 30 minute time limit, during the first to
second weeks in May for
the years 1994, 1995 and 1996. This was the pre-test.
5. I observed each resident's physical examination
in silence, checking off each of the
45 or 47 items as they were done, noting the starting and ending
times plus any
comments about the resident's performance.
6. Immediately after the test, I showed each
resident their check-list and explained
their deficiencies; also each resident received a photo-copy of
their check-list as
well as a copy of the University of Florida outline for physical
examination.
7. Each first year resident performed a repeat
physical examination check-list at the
end of the 6 month medical rotation. This is called the post-test.
The post-test was
similar to the pre-test in every way, except that the resident
choose the patient for
the check-list examination. The post-test occurred at the end
of the first 6 months for
half of the residents and at 12 months for the other half.
Physical Examination Skills
Results
I. Residents' characteristics
A. Number completing pre-test and post-test 22
(number not completing pre-test and post-test 2)
B. Age ~25
C. Sex 17 men, 5 women
D. Medical Schools 18 : 9 national, 1 city, 8 private
II. Quantatative results from check-list scores
A. Pre-test - Number of items checked
1994(n = 9) Mean 21 items (range 11- 30), or 47%
1995(n = 5) Mean 20 items (range 15 - 26), or 43%
1996(n = 8) Mean 20 items (range 13 - 30), or 42%(more female
breast exams)
B. Post-test - Number of items checked
1994(n = 9) Mean 37 items (range 28 - 44), or 84%
1995(n = 5) Mean 34 items (range 27 - 40), or 75%
1996(n = 8) Mean 39 items (range 34 - 44), or 85%
C. Total Pre-test (n = 22) Number of items checked Mean 20 items, or 44%
D. Total Post-test (n = 22) Number of items checked Mean 38 items, or 82%
E. Total Pre-test time used 16 minutes, or 55% of allotted time
F. Total Post-test time used 24 minutes, or 78% of allotted time
III. Qualitative impressions
A. Order of examination : Pre-test often erratic, Post-test improved
B. Technique : Pre-test often primitive percussion,
palpation and auscultation; Post-
test improved
D. Communication with patient : Pre-test poor, Post-test excellent
C. Frequently missed items : Pre-test many,
Post-test respiration rate, visual acuity,
ophthalmoscopy, hearing, otoscopy, breast(women), joints, mental
status,
coordination and gait
Physical Examination Skills
Comments
I. Recent medical school graduates(first year
junior residents) completed less than
50% of items while observed performing a physical examination
on adult in-patients.
2. After 6 months of internal medicine rotations, the first year
residents completed 82%
of items while observed performing a physician examination.
3. Although qualitative components were not systematically recorded,
most entering
residents had poor techniques of percussion, palpation, and
auscultation.
Post-test
techniques greatly improved.
4. Possible reasons for low scores during the pre-test
a. Inadequate training and practice in medical schools
b. Anxiety in performing physical examination observed by foreign
physician
c. Failure to use the allotted time
d. Small sample size, sampling errors, and bias of observer
e. PE check list not suitable for Japanese medical students and
residents
5. Possible reasons for improved scores during the post-test
a. Training and practice during internal medicine rotations
b. Using more of the allotted time
c. Studying the check list immediately before the post-test
d. Small sample size, sampling errors, and bias of observer
6. Comparisons with other Japanese residents: unknown
7. Comparison with American medical students not possible because
of major
differences in training and testing
8. Data from American medical schools for interest purposes only
a. University of Florida, Gainesville, requires 90% completion
of a 78 item check list
to pass the course; 0-2 fail each year ( 3 of 22 Kameda residents
had post- test
scores > 90% )
b. University of Hawaii, Honolulu, requires 95% completion of
a similar check list to
pass the course; none fail ( 1 of 22 Kameda residents had post
test scores > 95%)
Physical Examination Skills
Reflections
1. Japanese first year residents' physical examination skills are of questionable proficiency. Is this conclusion justified?
2. Japanese medical educators might want to replicate this study. If these finding are confirmed, Japanese medical educators might consider the significance of these finding. They also might want to consider improvements in the teaching of physical examination skills either in medical school, or in residencies.
3. Japanese medical educators further might consider detailed analysis of the skills of medical school graduates to perform a complete medical history, assessment and plan, the other components of clinical skills evaluation.
4. Although this audience is committed to improving medical students' clinical skills, perhaps the focus should be on ways to change medical school curriculum.
6. Stein, G.H.: Ideal skills for junior residents(JR). Proceeding: The 29th Japan Medical Education Society Meeting, Kanazawa, Japan, (July 1997).
Abstract
Ideal skills for Junior residents(JR)
Gerald H. Stein, MD, FACP
Kameda Medical Center (KMC), Kamogawa City, Chiba Ken
Ideal clinical skills for junior residents
include:
1. Development of the basic clinical skills for creative thinking
and solving clinical problems.
2. Integration of basic sciences of human diseases with clinical
medicine.
3. Interactions with senior residents, staff physicians, consultants
and department chiefs.
4. Learning to use medical literature search for clinical decisions:
evidenced-based medicine.
5. The development of life-long learning patterns.
6. Participation in peer review and quality assurance.
7. Community ethical focus.
Medical educators can teach the small steps
for JR to learn Problem Oriented System by insisting on a complete
listing of all problem and grouping the problems together to make
the assessments with a full differential diagnosis. The plan of
clinical studies follows logically from the assessment; no plan
is written without an assessment. The plan of treatment also follows
from the assessment. Teaching is done in small groups of JRs by
a detailed review of each entry into the patient's medical record,
with bedside visits to clarify history, expand review of systems
and demonstrate physical finding. Progress notes are similarly
fully discussed using the SOAP format. As the patient's hospital
course evolves, other skills are slowly introduced during chart
daily rounds. JR are encouraged to recall basic science components.
Differences of opinion between junior and senior residents, between
JR are consultants, between JR and attending physicians are encouraged
with proper evidence-based support from the medical literature.
Ethical issues such as Do-Not-Resusitate, informed consent, openness
with patients and their family about the illness are reviewed
as the clinical situation arises.
Examples from my teaching rounds will illustrate these points.
Conclusion: Medical educators and hospitals with JR programs might
want to study their goals. Such discussions might be helpful in
improving the clinical training programs in Japanese hospitals.
1. Development of the basic clinical skills
for creative thinking and solving
clinical problems
a. Problem Oriented System(POS)/ Subjective
Objective Assessment
Plan(SOAP) : Teaching in small groups by detailed review of each
entry
into the patients medical chart, with bedside visits to clarify
history,
expand review of systems(ROS) and demonstrate physical findings
b. Example of 1st year junior resident's medical
chart: 1st month
c. Example of 1st year junior resident's medical chart: 12th month
2. Integration of basic sciences of human diseases
with clinical medicine:
small group discussions with review articles
3. Interactions with senior residents, staff
physicians, consultants and
department chiefs: small group discussions
4. Learning to use medical literature for evidence-
based clinical decisions:
from library(books, journals, CD-ROM, Internet) to bedside
5. The development of life-long learning patterns:
attending physician as
role model
6. Participation in peer review and quality
assurance: quality improvement
by review of the residents own medical chart in small groups
7. Community ethical focus: small group discussions
as topic presents itself
from resident's patient.
Other manuscripts
7. Stein, Gerald H., Creative Thinking-Clinical Problem Solving Resident Physician Training program Kameda Medical Center. Japan Hospitals No 14, July 1995: 35-37.[Photocopy on request]
8. Stein, G.H., Clinical Rounds. URL: http://www2.gol.com/users/kmcdoc/; 1996-1999 [Photocopy on request]